Saturday, October 17, 2020
Monday, September 28, 2020
Dialysis Machine.
DIALYSIS
A normal kidney performs both filtration and cleaning process in the human body. It filters the impurities from the blood and removes extra toxins, excess water and other chemicals from the body. The kidney also helps in regulating blood pressure and other elements like sodium, potassium and bicarbonate in the body. It also provides vitamin D.
Dialysis is a procedure carried out in individuals having kidney failure (i.e a condition in which the kidney’s ability to remove toxins and excess fluid from the body fails). This procedure uses a machine to remove excess waste, fluids and salt from the body and to keep the patient’s body in balance.
Types of Dialysis
There are two types of dialysis
- Hemodialysis
- Peritoneal dialysis
Hemodialysis
Hemodialysis is the most commonly used method. This consists of an artificial kidney (dialyser) which removes wastes and excess fluids from the blood. During hemodialysis, the surgeon performs an operation to remove the blood from the patient’s body and allow it to enter into the dialysis machine. This artificial kidney purifies the blood and it is then returned back to the body.
Arteriovenous (AV) fistula is most commonly preferred for long term treatments. AV fistula is a surgical connection made between the artery and vein. Impure blood is removed from the surgical site through a catheter for filtration and purified blood is entered into the body.
If the blood vessel does not support adequate blood flow, then the surgeon connects a plastic tube or catheter for easier flow of blood. This type is known as the AV graft. Another method called vascular access catheter is also performed. In this method, the catheter is inserted into the large vein in the neck. The process of hemodialysis lasts up to 3 to 5 hours and it is done three times per week. It also depends upon the patient’s condition on how much waste is accumulated in the body. Patient’s must undergo hemodialysis in hospitals and dialysis centres.
Peritoneal Dialysis
Peritoneal dialysis can be performed by the individual at home. It consists of a dialysate, catheter and a drainage bag. The catheter is inserted into the peritoneum (a membrane covering the abdomen).
Dialysate is then passed through the catheter and it enters the abdomen. This dialysate absorbs excess waste and fluids from the blood and then it is allowed to drain. It gets collected in the drainage bag. This process takes only a few hours and is done five to six times a day. One can undergo this method even when sleeping or walking. Peritoneal dialysis is done to patients having acute renal failure which lasts up to a short span of time and recovers automatically.
Peritoneal dialysis is otherwise performed in three ways:-
1. Continuous ambulatory peritoneal dialysis (CAPD) – This method is performed several times a day. During this process, the patient must be awake. This method does not need any machine.
2. Continuous cycling peritoneal dialysis (CCPD) – In this method, a machine is used for sending the dialysate into the peritoneum and also for removing the drainage from the abdominal cavity. This must be performed only when the patient falls asleep.
3. Intermittent peritoneal dialysis (IPD) – This is similar to CCPD, but it takes a longer time and is performed in the hospital.
Risks of Hemodialysis:-
- It causes low blood pressure
- Anaemia
- Difficulty in sleeping
- Muscle cramps
- Bloodstream infections or sepsis
Risks of Peritoneal Dialysis:-
- A weakening of abdominal muscles
- Hernia
- Stomach pain
- Infections in the abdominal cavity
Deciding to Stop Dialysis
Before the conclusion, one must discuss with the doctor about stopping dialysis that he/she is undergoing. Without proper advice from the surgeon, one must not come to the conclusion because it may cause any serious harm.
Dialysis Machine
A Dialysis machine is a therapeutic device used in the process of dialysis for removing excess waste and for purifying the blood. Blood is removed from the patient’s body and is allowed to enter the dialyser (artificial kidney) in the machine. An anticoagulant (heparin injection) is present in order to prevent the blood from clotting. The dialyser is a semipermeable membrane which consists of dialysate( a mixture of water and electrolytes). Blood is purified in the dialyser and is pumped back to the body. Excess amount of urea and salt from the blood is removed by the dialyser.
The dialysate maintains the blood at a particular temperature. This is because a higher temperature will damage the blood components.
If the temperature rises in the machine, safety cut valve is used to switch off the heater. However, before allowing the blood to enter into the patient body, the blood is warmed by the heater. Therefore, the temperature is maintained between 36 – 42 degree Celsius. For controlling the temperature in the machine, it consists of a thermostat and a proportional controller.
This controls the power given to the heater. Pressure in the dialysis is monitored by the transducer. Negative pressure in the dialysate is created by the effluent pump. Therefore, if pressure raises, the effluent pump goes off. Dialysis machine also consists of a blood leak detector to monitor any leakage in the tubings or any other part of the machine. After completing the purification process, the used dialysate enters into the waste-collecting tank. Purified blood passes through the patient body.
Principle of Dialysis
The main principle of dialysis is based on diffusion and ultrafiltration.
In Diffusion, fluid flows from high concentration to low concentration through a semi-permeable membrane. In this process, impurities from blood diffuse into the dialysate, whereas electrolytes and other minerals diffuse into the blood from the dialysate. Therefore, purified blood is allowed to enter into the body and the dialysate is pumped out.
Ultrafiltration is the process of removing excess fluid from the body from positive to a negative pressure gradient (i.e high to low pressure). Here, blood comes under positive pressure, dialysate come under negative pressure.
Components& Functions of the Dialysis Machine.
- Blood Pump & Tubings – A blood pump is used to pump blood from the body to the dialysis machine
- Syringe – A drug called heparin is used in the injection. This is used to prevent blood clotting.
- Dialyser – Dialyser is also known as an artificial kidney. It is filled with a combination of water and electrolytes called dialysate. In this dialyser, blood is filtered and purified.
- Pressure Monitor – Arterial pressure monitor: This is used to detect the pressure between the blood coming from AV fistula and blood pump.
- Venous Pressure Monitor - This part usually measures positive pressure in the system. Low blood flow or any other disconnection in the circuit represents low venous pressure.
- Sensors – Sensors are used for monitoring various parameters in the circuit. This includes parameters like blood pressure, dialyser pressure gradient, temperature, Oxygen saturation etc.
- Air Detector – Air detector is used near the venous pressure line. This is used to detect any air leakage or the presence of any air molecules in the blood entering the patient’s body.
- Alarms – Alarms are used to prevent errors occurring in the functioning of the machine. This is used to detect blood flow, blood pressure, temperature, a mixture of dialysate.
Hemodialysis Catheter
A hemodialysis catheter is used to exchange blood from the patient to the dialysis machine. The catheter is of two types: with cuff and without a cuff. Catheter without cuff is used only for a shorter time (in peritoneal dialysis). The catheter consists of two openings. Red coloured opening indicates removing of arterial blood from the patient’s body into the machine. Blue colour indicates venous opening where purified blood is allowed to pass through the patient.
How to Prepare for Hemodialysis:-
Before performing dialysis treatment, the surgeon advises the patient to undergo a minor surgery called AV fistula or AV graft. This surgery is done before 3 to 4 weeks prior to the dialysis treatment. The time is given to heal the operated site. Vital functions of the patient’s body are also monitored during the treatment. They will monitor the height, weight, body temperature and other chronic conditions like blood pressure and diabetes are measured.
What Happens if There is a Power Failure During Dialysis:-
During a power failure, the dialysis machine stops working. Lights will turn OFF, and an alarm indicates power failure in the machine. The blood pump is operated by hand either to return the blood immediately or to keep the blood in circulation (incase if the machine gets power soon.) Once the blood is returned to the patient, the circuit must be disconnected. And the surgeon will ask the patient to come for another day. If the power is ON immediately after a power cut, the system will be able to resume the filtration process.
Problems and Troubleshooting:-
- Be sure to keep the machine clean and safe. Thoroughly clean the droplets, stains of blood as soon as possible to prevent infections.
- The person may be infected when operating the machine. So be careful when handling disposable products.
- Be sure the water, dialysate concentrate is good in quality in order to enhance performance and safety.
- Confirm whether all cable connections are correct and safe to prevent electric shocks.
- Do not operate the machine with wet or bare hands. Always use gloves to prevent infections.
Maintenance:-
- Calibration must be done regularly to the dialysate pump and blood pump.
- Preventive maintenance should be done to avoid equipment breakdown.
- Accurate timing must be maintained for ultrafiltration rate.
- Clean and disinfect the machine after using on each patient.
- Clean the machine from top to bottom using disinfectant cloths/wipes.
- Install the machine in a place where it is free from moisture
- Check the power supply
- Check the earth connections properly
Risks and Troubleshooting
Troubleshooting the machine should be done by qualified personnel.
👉 Watch Dialysis Machine Video from OurYouTube Channel Bolew:-
Article Prepared By:-
 |
| 👉 Sumitha Ramadass |
Reference
- https://www.healthline.com/health/dialysis#purpose
- https://www.kidney.org/atoz/content/dialysisinfo
- https://www.webmd.com/a-to-z-guides/kidney-dialysis#1
- https://www.pharmaceutical-journal.com/cpd-and-learning/cpd-article/dialysis-principles-and-treatment-options/20068038.cpdarticle?firstPass=false
- https://www.nephroxenia.com/de/post/1/aytologh-arthrioflebikh-anastomwsh
- https://www.nikkiso.com/products/medical/dialysis.html
- https://www.donate4hassan.org/blog/2018/8/20/peritoneal-dialysis-at-home
- https://www.assignmenthelp.net/assignment_help/principle-of-dialysis
- https://www.freseniuskidneycare.com/ckd-treatment/what-is-dialysis/hemodialysis-machine
- https://www.slideshare.net/tejabayapalli/hemodialysis-machine-62992148
- http://www.bcrenalagency.ca/resource-gallery/Documents/Cleaning%20and%20Disinfecting%20Hemodialysis%20Machines%20and%20Stations.pdf
- http://www.sjkdt.org/article.asp?issn=1319-2442;year=2009;volume=20;issue=1;spage=49;epage=56;aulast=Azar#:~:text=Routine%20preventative%20and%20annual%20maintenance,significantly%20impact%20adequacy%20over%20time.
- http://www.frankshospitalworkshop.com/equipment/documents/dialysis_units/service_manuals/Nipro%20Diamax%20Dialysis%20Machine%20-%20Service%20manual.pdf
- https://www.indiamart.com/meditech-devices-private-limited/meditech-dialysis-catheters.html
- https://www.kidney.org/atoz/content/hemocatheter
- https://science.howstuffworks.com/innovation/everyday-innovations/question17.htm
- https://www.slideshare.net/tejabayapalli/hemodialysis-62992175
Friday, September 25, 2020
Electro Surgical Unit (ESU).
Electrosurgery.
Definition:-
Electrosurgery is a procedure involved in cutting and coagulation of biological tissues. This procedure uses high frequency alternating electrical current. This is also used for dissection, fulguration (removal of abnormal tissue growth), and for shrinking tissues.
Principles of Electrosurgery.
The main principle of electrosurgery is that it uses an alternating (AC) electric current at high frequency or radiofrequency. The frequency ranges from 100KHz to 5 MHz. This current is passed through the patient’s body and produces the heat. Therefore, the surgical procedure is performed using an electrode and it is controlled either by a hand switch or footswitch.
Another procedure called Electrocautery is related to Electrosurgery. But in electrocautery, it uses direct current (DC) and heat is generated in the circuit, not in the patient’s body. Electrocautery is also known as thermal cautery. This procedure uses heated metal wire electrode for tissue destruction (i.e either to remove or coagulate the damaged tissue). As we all know, the movement of electrons is called electric current. In Direct current, electrons flow in the same direction. In Alternating current, the flow of electrons changes periodically.
Modes of Electro-surgery:
Monopolar Electrosurgery vs Bipolar Electrosurgery.
In Monopolar Electrosurgery, it consists of an electrosurgical generator, active electrode, patient and patient return electrode. During operation, the patient plate is attached to any part of the patient’s body. Electric current is generated from the electrosurgery generator and it passes through the active electrode where it creates heat in the tissue as well as the entire body cavity. And it returns back to the generator through the patient return electrode.
Monopolar is used to cut, coagulate, desiccate tissues. This is the most commonly used method in electrosurgery.
In Bipolar Electrosurgery, the bi-forceps electrode is used. The forceps perform both the active and return electrode function. Forceps are used for grabbing the tissue and the electric current passes through the forceps to the respective area in the tissue.
Therefore this prevents further damage to other body parts and prevents the patient from any burns. Bipolar surgery uses only less voltage and hence it is not used for cutting and coagulation of larger bleeding tissues. Bipolar surgery is recommended in patients with implanted devices to prevent them from short circuit.
Types of Electrosurgical Technique:-
- Electrocoagulation
- Electrodesiccation
- Electrofulgaration
- Electrocution
These techniques are used for destroying abnormal or damaged tissues. Also used to prevent loss of blood while performing the surgery.
Types of Current:-
There are three types of current used in electrosurgery
- CUTTING – Cutting current is a continuous sinusoidal waveform. The power of cutting current must be maintained between 50W and 80W. The surgeon holds the electrode slightly away from the tissue to create a spark for cutting. This spark creates heat in the tissue area.
- COAGULATION – Coagulation current is an interrupted and damped sine waveform. The waveforms have high peak voltages. Due to this, the temperature also increases causing thermal destruction in the tissues. Therefore, coagulating current is used for coagulation in bleeding vessels/tissues.
- BLENDING –Blend current has a combination of both cutting and coagulating current waveform. This is also a modified form of cutting current. This blending current is used in hemostasis of tissues. Blend current produces a higher peak to peak voltages. Therefore, the duty cycle also changes between the burst current and coagulation. For maintaining the same directional flow, this blend current can be rectified. Surgeries like dental and dermatology use rectified current.
Tissue Effects of Electrosurgery
- Vapourisation – Vapourisation of tissue is achieved by producing heat in the tissue. Heat is produced by creating a spark in the surgical area with the help of the electrode. During surgery, the surgeon creates a minimum spark over the tissue. Due to sparking, the maximum current can be produced.
- Fulguration –Fulgaration is a combination of sparking with coagulation. This creates longer sparks in the tissue. In this process, less heat is produced in the tissue. That is why coagulation takes place rather than vapourisation.
- Dessication – Desiccation is produced by low current density and high voltages. This is the modification of coagulation. In this procedure, the electrode is used directly in contact with the tissue, which converts the electrical energy into heat, which causes the cells to shrink.
Electrosurgical Unit
Electrosurgical unit is a device used in electrosurgery for cutting, coagulation, fulguration, and desiccation of tissues. Electrosurgical unit is used in surgeries to prevent blood loss. ESU consists of an electrosurgical generator with one or more electrodes and a patient return electrode. This unit is controlled using a hand switch or a footswitch.
The Electrosurgical Generator produces different waveforms corresponding to the tissue effects.
The Active Electrode is placed directly in the surgical area and the patient Return Electrode is kept in any part of the patient body.
The electrosurgical unit creates an electric current to pass through the electrode and produces heat in the tissue for cutting, coagulating and removing damaged tissues. It is operated under two modes: Monopolar and Bipolar.
In monopolar mode, there is an active electrode which carries the current to the tissue and a patient return electrode for taking back the current from the tissue. In bipolar mode, it uses the forceps type of an electrode which performs both active and return operations.
Electrosurgery is often similar to diathermy. Diathermy uses an electromagnetic current to produce heat. It uses dielectric poles. Diathermy passes electromagnetic waves and thus heat is generated in the body. The generated heat increases blood flow in the area causing pain. This is most commonly used in muscle and joint problems for allowing free blood flow.
There are three types of Diathermy. This includes:-
- Shortwave diathermy – High-frequency electromagnetic current is used to generate heat in the tissue. This is used to treat pains that occur during kidney stones.
- Microwave diathermy – Microwaves are used to generate heat in the body. Microwaves cannot penetrate deep into the muscles.
- Ultrasound diathermy – This uses sound waves by causing vibration in the tissues. This is used to treat deeper tissue areas.
Types of Electrodes
Block Diagram of ESU :
High-frequency power is required to generate heat from the waveform generator. Different waveforms like cutting, coagulation and blending are also produced from the generator. The mode selector is used for selecting which type of mode should be used while performing the surgery. Power level control determines the power applied to the electrodes during surgery. Alarm circuit is used for creating safety alarms whether the electrodes are attached properly in the patient circuit.
Circuit Components
The front panel consists of:-
Power ON/OFF switch – Turning On/ Off of the electrosurgical unit.
Mode selector – For selecting the modes for performing surgery (CUT mode, COAG mode, BLEND mode ). Cut mode indicates a yellow colour, whereas Coagulation mode indicates a blue colour.
Fault indicator switch – This indicates poor contact of patient return electrode with the patient by producing alarm. Three-pin switch for monopolar use only hand switch. Three-pin switch for bipolar can be activated with or without footswitch. There is also a two-pin connector for the patient return electrode.
Rear panel Consists of:-
Footswitch control – This is for connecting the footswitch.
The volume control knob - is used for controlling the audio volume during cutting, coagulation or blending. Power cord connection.
Safety precautions
- Electrosurgery must be performed by specially trained technicians in electrosurgical technologies.
- Electrosurgery should not be performed in oxygen-rich environments because it may easily catch fire and cause serious burns.
- Before operating, insulation of the electrode must be checked carefully to avoid thermal injuries.
- Do not activate the equipment in an open circuit.
Do’s
• Electrodes should be placed in clean, dry areas
• Use only insulated electrodes
• Electrodes must be placed in well-cleaned holster, when not in use
• Electrode tips must be cleaned properly.
• Use only low voltage waveforms while operating
• Bipolar electrosurgery can be performed when necessary
Don’ts
- One should not use the electrode in the presence of flame causing agents like (alcohol, tincture etc.) to avoid burns and fire.
- Electrodes should not be wrapped around metal instruments because they cause burns.
- Rubber catheters should not be used in electrode tips.
- One should not operate the electrosurgical unit by standing on a wet surface to prevent them from shocks.
- Surgeons or technicians must not perform the operation with wet hands/wet gloves to prevent electric shock.
- Must wear surgical masks during surgery to avoid smoking difficulties which may cause breathing problems.
- Avoid using the electrode near electric devices.
- Do not use the equipment in patients prior to testing.
Problems in ESU
• If surgery is performed in oxygen-rich environments, it may cause a surgical fire.
• Patient burns may also be caused by detachment of the electrode pad.
• Incorrect placement of the electrode may also cause burns.
• Electrosurgical injury occurs when the electrode comes in contact with non-target tissue.
• Since the device uses high current, it may cause electric shock, the transmission of infection etc.
• Direct skin contact will cause burns.
Preventive Maintenance
- Regular testing of the equipment should be done to prevent any harm and to enhance patient and staff safety.
- The person handling the equipment must be well trained by the manufacturer.
- He/She must follow the instructions given in the manual.
- The technician must carefully inspect the insulation.
- Lower power setting must be used when starting the equipment for use.
Risks of Electrosurgery
- Most of the risks are caused by thermal injuries. This is mainly due to unintended contact of the active electrode with any part of the body tissues.
- Another kind of thermal injury is caused by the contact of the active electrode with metal instruments.
- Injuries caused by smoke also causes breathing problems in both patients and surgeons.
- Major risks are associated with respiratory illness and irritation in the eyes, skin etc.
- Therefore, proper measures must be taken before handling the equipment during surgery.
Electrical safety
- The proper power cord must be used. It must be properly grounded.
- Use only proper fuses which have correct voltage and current rating.
Patient Safety
• Proper contact must be maintained between the patient and other metal parts to avoid burns.
• Patient electrode must be connected in order to avoid skin injuries.
• Ensure the connections made do not affect the blood supply in the patient.
Clinical Applications
- Electrosurgery is often used in most of the operations involving tissue surgeries
- ENT (To control nose bleeding)
- Gynaecology
- Ophthalmic surgery
- Dermatology (To remove abnormal skin growth, moles etc.)
- To remove lesions, hair follicles.
- Also used in surgeries associated with organs like liver, spleen, kidneys and heart surgery.
Environments of use
Electrosurgery is used in operating rooms in the hospital while performing surgeries.
Troubleshooting
- Check Electrosurgical unit for any physical damage
- Ensure all cables, electrodes, power cord is connected properly
- Check the power cord properly or immediately replace it.
- Pin connections and switches must be properly checked. If any damage is found, it must be replaced immediately.
👉 Watch ESU Video on Our YouTube Channel Below:-
Article Prepared By:-
 |
| 👉 Sumitha Ramadass |
References
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3407433/#:~:text=Principles%20of%20Electrosurgery,Often%20%E2%80%9Celectrocautery%E2%80%9D%20is&text=Electrocautery%20refers%20to%20direct%20current,alternating%20current%20(Figure%201).&text=Electrical%20current%20flows%20when%20electrons,produced%20when%20electrons%20encounter%20resistance.
- http://www.boviemedical.com/2016/10/03/bipolar-electrosurgery-vs-monopolar-electrosurgery/
- https://www.asit.org/assets/documents/Prinicpals_in_electrosurgery.pdf
- https://www.glowm.com/section_view/heading/electrosurgery-principles-biologic-effects-and-results-in-female-reproductivesurgery/item/21#:~:text=There%20are%20three%20basic%20types,%2C%20nonmodulated%20sinusoidal%20waveform%20(Fig.
- https://veteriankey.com/surgical-modalities-laser-radiofrequency-ultrasonic-and-electrosurgery/
- https://www.semanticscholar.org/paper/Electrosurgery%3A-principles-and-practice-to-reduce-Brill/ba1a6e6b411cba18601762375b62562cdf166677/figure/5
- https://www.uptodate.com/contents/overview-of-electrosurgery
- https://www.slideshare.net/prasadvagal/electrosurgical-unit
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4579996/#:~:text=An%20electrosurgical%20unit%20(ESU)%20consists,do%20the%20corresponding%20tissue%20effects.
- https://avantehs.com/p/11947
- https://www.cehjournal.org/article/electrosurgical-units-how-they-work-and-how-to-use-them-safely/
- https://www.gimaitaly.com/prodotti.asp?sku=30512&dept_selected=44&dept_id=446
- http://www.micromed.com/en-US/products/electrodes/
- https://www.sutter-med.de/en/products/monopolar-instruments/monopolar-electrodes_aid_50.html
- https://www.who.int/medical_devices/innovation/electrosurgical_unit.pdf
- https://www.flukebiomedical.com/blog/what-are-electrosurgical-units-why-should-we-test-them%3F
- https://webstor.srmist.edu.in/web_assets/srm_mainsite/files/downloads/esu.pdf
- https://www.magmedical-equip.com/product/valleylab-force-fx-c-electrosurgical-unit/
- https://docplayer.net/21481453-Instructions-electrosurgical-unit-psd-30.html
Wednesday, August 26, 2020
Infusion Pump
Introduction
An infusion pump is a medical device which is used to deliver a large or small amount of fluid to the patient’s circulatory system with or without nutrients or medications in a controlled format. It is commonly used intravenously. There are several infusions which are used intermittently such as subcutaneous, epidural and arterial infusions. Commonly used infusion pumps are intended for some specialized purposes as follows:
- Enteral pump - The pump is used to deliver liquid nutrients and medication to the patient's digestive system.
- Patient-controlled analgesia (PCA) pump - A pump used to deliver pain medications, which is equipped with a feature that allows patients to self-administer a controlled amount of medication as needed.
- Insulin pump - A pump is often used to deliver insulin to patients with diabetes. Insulin pumps are often used at home.
What is Injection & What is Infusion
An injection is a procedure of placing a liquid, mainly a drug, into the patient’s body by using a needle (generally a hypodermic needle) and also a syringe. This is a technique for delivering drugs by the parenteral administration, which is, the administration through a route other than via the digestive tract. This parenteral injection including following injections such as:
- Subcutaneous injection
- Intramuscular injection
- Intravenous injection
- Intraperitoneal injection
- Intraosseous injection
- Intracardiac injection
- Intraarticular injection
- Intracavernous injection
The following figure shows the four types of angles of the needle insertion for the following four types of injections:-
- Intramuscular injection
- Subcutaneous injection
- Intravenous injection
- Intradermal injection
 |
Figure – Angles of needle insertion |
Infusion is suffusing/ infusing of liquid substances directly into a vein using an infusion pump. These infusions are administered intravenously including in the designation of the speciality of drugs. Infusion also time controlled. It is normally referred to as a drip and many systems of the administration utilize a drip chamber, which prevents the air from entering the bloodstream (air embolism), and it allows an evaluation of the flow rate.
Comparison with the other routes of the administration, and to deliver medications and fluids throughout the body, the intravenous route is the fastest way. The bioavailability of the medication is 100% in IV therapy.
Infusion is used to deliver to the patient following things:-
- Blood
- Electrolytes
- Water
- Drugs
- Nutrients
- Other fluids
 |
| Figure – Infusion of medication with the infusion IV set |
Differences (Comparison between Injection and Infusion)
There are some comparisons:-
- An injection doesn’t require any IV lines, nor does it require an IV pump.
- Injections are an effective way to administer medication.
- Infusions are much more similar to traditional IV drips.
- An infusion is typically used to treat some type of chronic issue such as pain.
- Infusion is well time controlled and able to deliver the medication in a period of time.
What is Intravenous (IV) Therapy?
Intravenous (IV) therapy is a therapy in which fluids are released directly into a vein. The intravenous route of administration can be used for both injections using a syringe at higher pressures; and for infusions, using only the pressure provided by gravity. Intravenous infusions are commonly known as drops.
The intravenous line is the fastest way to administer medications and replace fluids throughout the body because they are introduced directly into the circulation. Intravenous therapy can be used to replace fluid volume, correct electrolyte imbalance, for the medication manager, and for blood transfusions.
 |
| Figure – Intravenous IV therapy |
What is Infusion Therapy
An exceptional to oral therapy is the infusion therapy: administration of injection with an antiseptic catheter. Traditionally, this technique has only been used inside the hospitals, but also infusion therapy is possible to be performed by specialist nurses in outpatient clinics or even at home by the present. These nurses are licensed by the State Pharmaceutical Board and meet authoritarian standards and the regulations which are set by the Board of Directors and government.
 |
| Figure – Infusion therapy. |
What Does Infusion Therapy Treat?
The infusion therapy is generally used to take care of severe or any chronic infections which do not retort to oral antibiotics. Cancer and the cancer pain; Gastrointestinal diseases; Dehydration from vomiting, nausea, and diarrhoea. And the other serious illnesses like Crohn's disease is common. Other complex diseases that retort better to intestinal disorders including multiple sclerosis, certain arthritis, cardiovascular disease, and certain immune responses. Some cognitive disorders also require rashes.
Why we need infusion therapy
We need this, to not just oral medications when people who are seriously ill sometimes can't eat. Also, some actions cannot be taken orally, for the reason that stomach acids kill them and are no longer valuable & effective in treating your disease.
Examples/Types of infusion therapies
• Anti-Coagulation Therapy
• Blood Component Stimulating Factor
• Chemotherapy
• Hydration
• Anti-Hemophilic Factors
• Anti-Emetics
• Enteral Nutrition
• Pain Management
• Total Parenteral Nutrition
• Inotropic Therapy
History
The first attempt of intravenous medicine has been recorded in 1492. And it was invented the very first IV infusion pump device by Christopher Wren who was a famous architect in 1658. Then after seven years in 1665, it was carried out the first successful blood transfusion. During the intravenous procedures, it was invented the infusion pump prototypes controlling the flow rate in the 19th century.
It was able to see the huge advances of infusion pumps in the 20th century.
- Dean Kamen was able to do some major developments of the infusion pump in the 1970s’.
Types of the Infusion pump
There are three types of the infusion pumps according to IEC 60601-2-24 international standard as follows.
 |
| Figure – Types of infusion pumps |
1. Volumetric:-
With infusion pumps (volumetric), the mechanical trigger sources the fluid in the tubing to move through a peristaltic effect that allows medication and nutrients or foods to be distributed. This mechanism could be categorized as rotating or linear.
The mechanism of rotary is made of the main rotor and entire with rollers that pressing the tube.
 |
| Figure - Rotary peristaltic pump |
The linear mechanism is the most common type and consists of several independent fingers pressing sinusoidal on the silicon tube and these fingers perform the peristaltic movement and force the river to pass by pressing infusion line in opposition to the orifice of the device.
 |
| Figure - Linear peristaltic mechanism |
This mechanism is stimulated by a stepper motor with reduction gear and also managed by an electronic circuit that shows on the screen the stream and also the amount of liquid to be identified delivered most linear and rotating infusion pumps (volumetric) have the drop sensor, an inline air sensor and occlusion pressure sensors.
 |
| Figure - Several types of volumetric infusion pumps. |
Infusion pumps aspired at enteric nourishment have a mechanism identical to that of as described above. However, they are simple and haven’t any drop sensors and manage an uttermost pressure sensor.
2. Infusion Pumps with a Syringe:-
The pump system consists of an exterior electronic pump, an infusion of the line and syringe are companionable with this system and are generally disposable. The companionable syringe is a device that meets the specifications and requirements specified in recommendations of the manufacturer's.
 |
| Figure – Pump system of the syringe. |
A disposable syringe is inserted into the pump for holding it, packed with a prescribed medicine fluid. Then this piston is mounted on a support and this equipment is programmed. It is sprayed manually or automatically. The injection pump automatically adjusts to the syringe connected to the equipment.
 |
| Figure – Syringe infusion mechanism |
Syringe pumps are able to be used independently or else in a multi-channel system. There are two types of configurations for multichannel systems, such as two or more individual pumps which are programmed from a general control panel, and separate module controlling two or more individual pumps which are connected to the side of the system.
 |
| Figure – Examples of syringe pumps |
Elastomeric infusion pumps are usually used for pain relief, in the stack or in the hospitals. In these kinds of pumps, the infusion pressure is gained by filling or satisfying the elastic balloon and also the flow control is done by the pressure disparity produced by the body temperature.
Main Parameters:-
Infusion pump has four major parameters such as volume, flow, time, and pressure.
The intention of the parameter of the volume is to evaluate the virtual values related to the volume applied. The volume to be administered should be based on the total amount of liquid available in the reservoir and it is recommended that it be between 0.1 ml and 0.1 ml 9999.0 ml. The delivery volume is that of the pump at the closing stages of the administration and it is not programmable. Corresponding to the total amount of used fluid.
The infusion time is the time interval in that the liquid is administered. The parameter can be programmed relevant to the respective requirements, such as Medicine administration. The pumps are programmable in seconds, minutes and hours.
The parameter related to the flow is the volume of liquid administered over a long period of time.
Time although most infusion pumps are delivered in millilitres per hour (ml / h). Volume flow: some can be programmed to provide mass in milligrams per hour (mg / h). Fluid The flow control can be volumetric or non-volumetric and the programming of the standards should be restricted to the measurement range of the instrument. In terms of flow, it is essential to mention that the bolus parameter, which is to supply a convinced amount of liquid in a short period of time.
Evaluation of the parameter applied to the pressure of the infusion pump, especially when monitoring the supply pressure that can be generated by the pump when there is a liquid lock in the system.
Main Components:-
There are the following components of the infusion pump.
1. Alarm
2. Control circuit
3. Infusion line & accessories
4. Infusion mechanisms
5. Display and control panel
6. Motor
7. Drop sensor in peristaltic pump
8. Air sensor inside the peristaltic pumps
9. Occlusion pressure sensor
10. Keypad
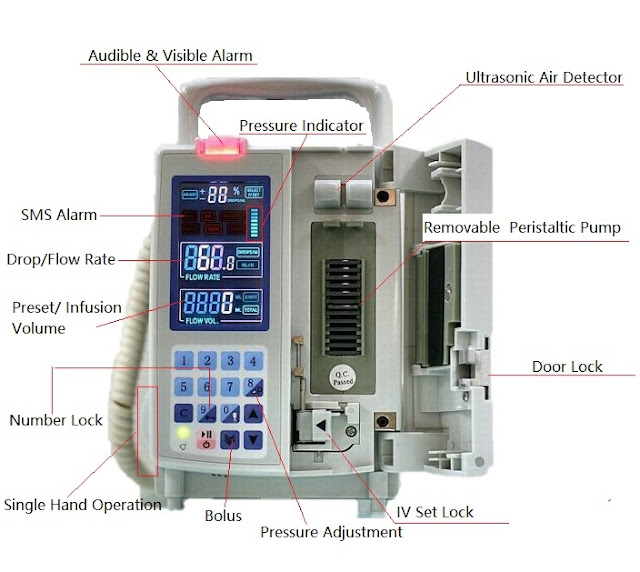 |
| Figure – Components of the infusion pump |
The following table illustrates the function of the above mentioned each and every component of the device.
 |
Figure
– Table of the function of the components |
Accessories of the Device
There are accessories of the infusion pump which are important in deliver fluids as follows:-
1. Lines / Extensions.
These extensions also known as IV tubes are in different dimensions of lengths & diameters. These lines are unidirectional extensions and consists of valves in order to prevent from returning.
2. Needle.
This needle is used to guarantee & puncture the admittance
to the blood vessels.
3. Catheter.
4. Valve.
5. Filter
Filters can be antibacterial. Its function is to remove waste, prevent contamination, and prevent air bubbles from reaching the patient. To perform these tasks effectively, it is recommended to use the filter once in a clinical setting.
Working Principle
These pumps are controlled by a microprocessor. Peristaltic pumps sequentially compress and release the infusion tube, which injects fluid into the patient's catheter. The speed of a stepper motor determines the cycle speed of the peristaltic mechanism that controls the infusion rate. These pumps offer a flow rate of 0.01 to 999 ml/hour. Syringe-based pumps use a syringe as a reservoir for the drug that drives the liquid, pushing the plunger into the body of the syringe. A lead-screw mechanism presses a thread block against the piston. Spray regulators use spring or gas mechanisms to provide relative care constant force on the piston, which creates constant pressure for the fluid supply.
Operating Steps
- Patient’s skin should be cleaned by using alcohol and then the infusion site is fixed with the catheter port that is connected to the infusion pump.
- An appropriate solution fills inside the reservoir.
- It has been programmed to deliver/send a specific quantity of volume at a specific rate.
How It Works….
- Attach the IV tube to the saline bottle and fix an IV tube in the peristaltic sheet, then close the door of the pump
- Tap the switch which is situated behind equipment & start the machine.
- According to the requirement set the mode as adult or pediatric.
- Set the mode button of the unit of the volume.
- Depend on the several models of infusion pump you can then set as the next step, by setting the specific volume in specific time to be automatically calculated the rate and display on the screen and or can set directly set the rate.
- After finishing all these settings press the start button to start infusing the medication liquid.
- For infusing liquid at fast you can use the ‘BOLUS’ option. (BOLUS option - Clinically, the bolus is the administration of many drugs, drugs, or other drugs over a long period of time, usually for 1 to 30 minutes, to increase blood pressure in the blood.
- When you need to stop infusing medication you can press the STOP button.
Block Diagram of the Infusion Pump
 |
| Figure – Block diagram of the infusion pump |
This diagram provides a scalable platform which integrates all the required circuitry to provide a configurable Infusion Pump in a single chip, including the followings:
- The high precision Analog front end, including a 0.1% accurate Voltage reference and up to 20 bits of resolution
- Circuitry for controlling the Relay Valve for controlling the flow rate and flow uniformity
- LCD direct-drive and control
- Power management capabilities including Battery Charging and Protection, Fuel Gauge, and Voltage Sequencing / Monitoring.
- On-chip EEPROM
Maintenance of the Device.
- To reduce and eliminate errors, maintenance takes everyone into account, the preventive and corrective measures essential for the proper functioning of the equipment and all their components. An object is understood to mean "every element, every part, apparatus, subsystem, instrument, functional unit or system that can be viewed separately.
- In this perspective, the inspection, clean-up and the replacement of each part are used and is relevant in the context of best practices. Conversely in order to determine the appropriate maintenance frequency for each and every infusion pump, and the following also should always be taken into account: the recommendations of the manufacturer, and the utilization of the device. Visual inspection and cleaning requirements must and should be performed daily.
- This is important regardless of the basic principles emphasize that preventive maintenance work must correspond to the measures and the specifications described by the device manufacturer are intended to prevent this. An error occurs that increases the average time between them. In this way, it is possible to guarantee maximum consistency and operational availability. Under the conscientiousness of the owner of the equipment plans are also preventative maintenance and if necessary, the components must be replaced during maintenance.
- The visual inspection consists of an evaluation of the general conditions of the infusion pump, that is the inspection of the casing, the piston, drop sensor, power cable, the keyboard, power cable, the battery, doors, and hinges. In addition, the operational status of the alarms is verified, not only the audio that will be heard but also the visual part of the illuminated signal LED.
 |
| Figure - Visual inspection of an infusion pump (volumetric): lateral verification (on the left); Frontal (in the centre) and verification of the drop sensor (on the right). |
 |
Figure - Visual inspection of an infusion pump (volumetric): exterior and interior door (on the left) and drop cable sensor (on the right). |
Good Practices
The manufacturer's safety instructions and instructions in the appropriate regulations must be followed to utilize the infusion pump safely. It is significant to note that internationally, there are numerous documented security incidents consisting of patients related to the use of this type of equipment. Mainly due to human error or defective equipment/consumables/accessories
The followings show the considerable good practices of uses:
Safety of the Instrument
- Assuring the preventive maintenance.
- Identifying the equipment has been attached to a label which shows the resistant for decontamination.
- Identifying the equipment states of the maintenance also the calibration
- Decontamination of the equipment according to the manufacturer’s guidelines.
- Prevention of the risk of the explosion, by not using any the flammable products near to the equipment.
Safe Handling
- Transportation of the equipment safely with sustain devices consists of wheels.
- Install the device in place and store it in a safe place so that it does not hit the patient if it falls.
- Use consumables/ accessories which are similar in temperament with the equipment.
- Avoid, the admittance to the arrangement of commands of the equipment, of avoiding risks of handling by the non-authorized persons.
- Avoiding of use of the pump in the battery mode and option to electrical extensions
- Minimizing the errors of handling consumables for standardizing the use of the equipment.
Storage
- Avoid the equipment from humidity and store it at a safe place.
- To charge the batteries of the equipment, make sure there are sufficient electrical outlets to be connected.
Technical Aspects to be Considered
- It is recommended to use syringes with a rigid volume and a reduced volume also shorter lines with the smaller inner diameters to minimize the effect of delayed liquid dosing, especially at flow rates of less than 2 ml / h.
- At very low flow rates (e.g. 0.5 ml/hr), normally used in the neonatology, and the conditions of utilizing should be parallel to those specified for calibration procedures to ensure that instrument error is reproducible under conditions. liquid viscosity and pressure.
- When utilizing multiple syringes on the same line, the effect of dead volume on the variation of the programmed flow of each syringe must be taken into account. This interaction between different pump infusions can lead to variation in doping error. Therefore, devices must be used to reduce the dead volume and reduce the reaction time of pumps.
Safety of the Instrument
- Assuring the preventive maintenance, also the functions that guarantee the relevant Metrological traceability;
- Identifying the instrument with a label which is opposing to the decontamination;
- Identifying the instrument’s state of the maintenance and the calibration;
- Decontaminating the instrument according to the instruction of the manufacturer;
- Preventing the risk of the detonation, by not using the instrument in a flammable environment.
Safe Handling
- Transporting the equipment securely with supportive devices which have wheels;
- Fixing the instrument in use, protecting it in a safe place so it will not strike the patient in case it falls;
- Using the consumables which are companionable with the instrument, in conformity with the specifications of the manufacturer. Normally, syringes which are different from the ones recommended by the manufacturer have a different internal diameter to the one programmed in the pump. This can lead to a significant error in the dosage of the fluids.
- The case presented in the Best Practice Guide exemplifies this situation (Lucas et al., 2015): a variation of 5 % in the diameter of the syringe can result in a flow error above 10%
- During the installation of the IV infusion set, verify if the referred and programmed dimensions in the pump are satisfactory;
- Block, if possible, the access to the configuration commands of the equipment, in case there is the risk of it being handled by non-authorised people (for example children or confused patients);
- Avoid using the infusion pump in battery mode and resorting to electrical extensions;
- In order to standardise the use of the instruments, they should be of the same model. In this manner, the errors in handling and in the utilisation of consumables are minimised;
- Place the configurations and the total amount of records to zero or to default values after using the devices/equipment as well as before its storage.
Infusion Pump Errors
Software problems:
If a software error message is shown, circumstances that the pump is inoperable at the moment. This happens in the absence of an identifiable problem.
Battery failures:
- A design concern causes overheating of the battery and the leads to premature battery failure.
- The battery is not replaced during the recommended according to the manufacturer’s guidelines to end of life routine maintenance.
Alarm errors:
- If there is a critical problem in the infusion pump such as occlusion (Clamped tubing) or else, presence of air in the infusion tube, the alarm alert fails to provide.
- Sometimes the device generates an occlusion alarm when the absence of an occlusion.
- Different alarm alerts of the infusion pump
 |
Table – Different alarm alerts of the device |
Broken components:
The device might have been damaged during the utilize, which may result in an over-infusion or an under-infusion if the pump keeps on being used without being repaired.
Fire or sparks:
- The user plugs in or unplugs the equipment from an electrical outlet and obtains a spark.
- According to the following figures may be noted a burning smell or flames on the infusion pump.
Troubleshooting
👉 Watch Our YouTube Video on Infusion Concepts below (Part 1):-
👉 Watch Our YouTube Video on Infusion Pump below (Part 2):-
References
- Alexander, M., Corrigan, A., Gorski, et. al. (2010). Infusion Nursing: An Evidence-based Approach. 3rdEdition. Saunders Elsevier.
- Association for the Advancement of Medical Instrumentation (AAMI) & US Food and Drug Administration (FDA). 2010. Infusing Patients Safely Priority Issues From the AAMI/FDA Infusion Device Summit. URL:http://s3.amazonaws.com/rdcmsaami/files/production/public/FileDownloads/Summits/A
- AMI_FDA_Summit_Report.pdf. Consultado em 2016-10-16. BATISTA, E., BISSIG, H., PETTER, H., et al. (2015). Primary standards for measuring flow rates from 100 nl/min to 1 ml/min – gravimetric principle. Biomedical Engineering, de Gruyter, 60:4.
- ISO 3696:1978. Water for analytical laboratory use -- Specification and test methods.
- Timmerman, A., Snijder, R., Lucas, P. et al. (2015). How physical infusion system parameters cause clinically relevant dose deviations after set point changes. Biomedical Engineering, de Gruyter, 60:4.
- Lewin, Ch. (2016). Precision Fluid Handling. Performance Motion Devices. URL: https://www.pmdcorp.com/resources/case_studies/4#. Consulted on 2017-03-30
Article Prepared By:-
Subscribe to:
Comments (Atom)




























