The amount of arterial gases, such as oxygen and carbon dioxide, is measured in an arterial blood gas (ABG) test.
In whole blood specimens, analyzers are utilized to assess blood gas, pH, electrolytes, and certain metabolites. They can measure pH, carbon dioxide, and oxygen partial pressures, as well as the concentrations of a variety of ions (such as sodium, potassium, chloride, bicarbonate) and metabolites (e.g.: calcium, magnesium, glucose, lactate).
ABG analysis is also used to detect acidosis and alkalosis conditions, kidney and lung function, response to treatment, and acid-base balance in the body.
What is an ABG machine?
An ABG (Arterial-Blood Gas) machine, also known as Arterial-Blood Gas Analyzer, is used to measure the amount of oxygen and carbon dioxide (called blood gases) in the blood. It is also used to determine the blood pH (Power of Hydrogen).
What is a Blood gas Test?
The amount of oxygen and carbon dioxide in the blood is measured by a blood gas test. It can also be used to determine the pH, or acidity, of the blood. A blood gas analysis or arterial blood gas (ABG) test is the most popular name for the test. Throughout the body, red blood cells deliver oxygen and carbon dioxide. They are known as 'Blood gases'. When blood travels through the lungs, oxygen enters the bloodstream, while carbon dioxide exits the bloodstream and enters the lungs. The blood gas test can show how successfully the lungs exchange oxygen into the bloodstream and eliminate carbon dioxide from the blood.
Why is the ABG machine used?
- The ABG machine is used to diagnose several breathing and lung conditions such as chronic obstructive pulmonary disease (COPD), or cystic fibrosis (a life-threatening hereditary disorder that affects the lungs and digestive system).
- To check if the blood requires extra oxygen or any assistance with breathing.
- To check the acid-base balance present in the blood. There can be too much acid in case of kidney failure, infection, or any toxic component intake.
- To monitor whether and how the lungs are responding to treatment.
- To monitor if the lungs are removing the right amount of carbon dioxide (CO2).
- To monitor vital kidney functions.
- To find the presence of respiratory acidosis, respiratory alkalosis, metabolic acidosis, or metabolic alkalosis.
How does the ABG machine work?
- At 37°C, blood gas analyzers have three electrodes that measure pH, PCO2, and PO2. They were first introduced in the 1960s, after innovations by R Stow (CO2) and L Clark (PO2) in 1954.
- Electrodes are used in blood gas/pH analyzers to determine pH, carbon dioxide partial pressure, and oxygen partial pressure in the blood.
- A dry reagent pad system is used in chemistry analyzers, in which a filter pad impregnated with all of the chemicals required for a certain reaction is placed on a thin plastic strip.
- The ion-selective electrode (ISE) approach is used in electrolyte analyzers, in which measurements of ion activity in a solution are made potentiometrically using an external reference electrode and an ISE with an internal reference electrode.
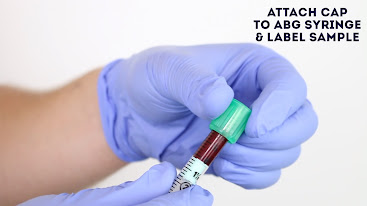
How is blood prepared for an ABG test?
The only anticoagulant used to prepare blood samples for blood-gas analysis is Heparin. Inadequate anticoagulation and the production of tiny blood clots, which can block the sample stream of blood gas analyzers and invalidate results, are two of the most common practical difficulties associated with blood gas analysis.
Whole blood samples are put into the analyzer in tubes, reaction cuvettes (a piece of laboratory equipment designed to contain samples for spectroscopic analysis), syringes, capillaries, or test strips. It is critical to remember that no blood should be injected or poured into the machine. Using a keypad or a linked computer, the operator can pick the tests that will be performed on the sample.
Where is the ABG machine used?
Hospital, patient bedside, physician's office, clinical laboratory, and home are some of the places where this device is used.
How is the blood drawn for the ABG test?
Blood is usually drawn from an artery. Blood from a vein may be used in some instances (venous blood gas).
Blood is most typically drawn from one of the following arteries:
• The radial artery (wrist)
• The brachial artery (arm)
• The femoral artery (groin)
Before collecting a blood sample from the wrist area, the health care professional may do a circulation test, also known as Allen Test (a test that determines whether or not the blood flow to the hand is normal. For a few seconds, the health professional drawing blood will apply pressure on the arteries present in the wrist. The blood flow to the hand will be cut off temporarily, and the hand will turn cool and pale).
A tiny needle is inserted through the skin into the artery by the provider. The sample is sent to a laboratory for analysis right away.

What are the main components of an ABG?
There are six main components to an ABG. They are as follows:
1. pH
2. Oxygen partial pressure (PaO2)
3. Carbon dioxide partial pressure (PaCO2)
4. Bicarbonate (HCO3)
5. Oxygen saturation (O2 Sat)
6. Oxygen concentration (O2 CT)
What are some of the body conditions that require ABG analysis?
The ABG machine is used to diagnose several breathing and lung conditions. Some of the common conditions ABG is used for are:
1. Respiratory acidosis:
Inadequate alveolar ventilation causes respiratory acidemia (acidosis), which results in the retention of carbon dioxide and an increase in free hydrogen ions. It happens when reduced breathing (hypoventilation) raises the concentration of carbon dioxide in the blood and lowers the pH of the blood.
2. Respiratory alkalosis:
Respiratory alkalosis is caused mainly by excessive carbon dioxide excretion/exhalation (hyperventilation), which results in the exhalation of more CO2 than is normal. As a result, the number of free hydrogen ions decreases, resulting in an alkaline condition.
3. Metabolic acidosis:
Excess fixed acid production, such as lactate or HCO3 loss, is a symptom of metabolic acidosis. It occurs when the body produces too much acid or when the kidneys do not remove enough acid from the body. Acidemia (acidosis) is characterized by a low blood pH (7.35) caused by the body's excessive production of hydrogen ions or its inability to produce bicarbonate (HCO3) in the kidneys.
4. Metabolic alkalosis:
Metabolic alkalosis is caused by a decrease in hydrogen ion concentration, which leads to an increase in bicarbonate, or is caused by increased bicarbonate concentrations.
How are the ABG results interpreted?
The pH should be checked first to see if the patient is within normal range, above the normal range, or below the normal range. A patient is in alkalosis if his or her pH is more than 7.45. If the pH is below 7.35, the patient is in acidemia (acidosis). Remember that the lower the pH number, the more acidic the body is. Even though the pH is normal, acidosis or alkalosis may still exist since the body can compensate to keep the pH balanced.
After that, examine the PaCO2 level. This will reveal if the variations in blood gas are caused by the respiratory system or by metabolic alterations. The medical expert will be able to fully interpret the blood gas when combined with the HCO3.
Below is a table to help in better understanding of ABG results interpretation:
ABG | pH | PaCO2 | HCO3 |
Respiratory Acidosis |
Low
|
High | Normal |
Respiratory Alkalosis |
High
| Low | Normal |
Metabolic Acidosis |
Low
| Normal |
Low
|
Metabolic Alkalosis |
High
| Normal |
High
|
· What are the normal ABG values?
pH | 7.35-7.45 |
pCO2 | 35 mmHg – 45 mmHg |
pO2 | 75 mmHg – 100 mmHg |
HCO3- | 22 mEq/L – 26 mEq/L |
O2 Saturation | > 95 % |
*mEq/L – milliequivalents per litre *mmHg – millimetre of mercury
The normal value varies depending on the laboratory, machine model, and age factor (for example, infants may show different normal values compared to the elderly).
What are the risks associated with ABG?
A blood sample collected from an artery has a low risk of causing complications. Although sometimes, any test that requires the use of a needle entails the risk of bleeding, infection, and bruise. There may be some tenderness/soreness where the needle was inserted.
- There could be a tiny bruise on the affected area. It is advised to apply pressure on the location for at least 10 minutes after the needle is removed to reduce the risk of bruising.
- A nerve or an artery may be damaged by the needle in rare situations. The artery may become blocked as a result of this.
- When the process is performed appropriately, there is very little risk. The size of veins and arteries differs from person to person and from one side of the body to the other. It may differ because drawing blood from some patients can be more difficult than from others.
Other concerns of having blood drawn are minor, although they can include:
- Feeling faint or lightheaded
- Several punctures are used to locate blood vessels.
- Hematoma - a type of hemorrhage (blood build-up under the skin)
- Excessive loss of blood
- Infection
What is the cost of an ABG machine?
In India, the price of an ABG Machine typically ranges from INR 3 lakh to INR 7 lakh.
What are the advantages of an ABG machine?
These ABG systems provide a number of advantages, including
- Less maintenance,
- Improved fault detection, and
- Reliable quality control.
Another benefit is a reduction in phlebotomy-related blood loss, which is critical in settings such as the operating room (OR) or intensive care unit (ICU), where blood conservation is critical. Analyzers are becoming faster, smaller, and more user-friendly, and they are demonstrating the potential to perform accurate testing with smaller blood samples.
What are the disadvantages of an ABG machine?
- One of the disadvantages includes a sample being mishandled or testing performed wrong.
- In a hospital, emergency department, or big clinical laboratory, qualified healthcare providers perform blood gas analysis.
These tests are "stat" tests, which means they should be completed as soon as possible after the sample has been collected. The obtained blood sample for arterial blood gases (ABGs) degrades rather quickly. Therefore, if a testing delay is anticipated, the sample should be maintained on ice and rewarmed later for accurate analysis. If any air bubbles remain in the top of the syringe after the sample has been collected, they must be removed. The syringe is then placed on ice and transferred for quick analysis when the needle is sealed.
Some instances of the sample being mishandled are:
If the sample contains air bubbles.
If the sample gets contaminated with venous blood.
If the blood sample coagulates due to insufficient heparin coating of the tube.
If there is an excess of heparin (liquid heparin will dilute the blood and cause changes in the pH value, leading to wrong value display).
Occurrence of hemolysis before the sample being placed in the ABG analyzer.
Another disadvantage could be a lack of proper documentation, leading to the loss of important patient details.
What are the instrumental errors that can occur in an ABG machine?
- The inaccurate temperature of electrolytes.
- Improper calibration of ABG analyzer
- Inadequate quality control and electrode maintenance (electrodes have various measurable lifespans).
- Poorly compensated non-linearity of the Clark electrode.
*(CLARK ELECTRODE - a well-known sensor for measuring dissolved oxygen concentration in a water solution. This type of electrochemical sensor has the advantage of being easy to detect extremely low oxygen levels. This electrode needs to be replaced once every 3 years as its Teflon membrane becomes coated with proteinaceous filth).
How to troubleshoot instrumental errors?
Ensuring proper maintenance of the machine:-
Frequent and adequate calibration of ABG analyzer. Calibration is a procedure performed on blood gas electrodes prior to testing blood samples to ensure that readings are accurate within the expected range.
Gases used for calibration should be exceedingly precise and able to be traced back to certification from the National Institute of Standards and Technology (NIST):-
Initial adequate Quality control checking of the machine and its parts.
When it comes to blood gas electrodes, quality control is monitoring the instrument's performance on a regular basis to ensure calibration, stability, and reliability.
The accuracy and precision of blood gas measurements are assessed using statistical approaches.
The most controllable part of quality assurance is certainly quality control.
• The lifespan of the machine should be considered and appropriate measures should be taken.
• Internal quality control processes are meant to ensure that a laboratory's instruments
(e.g., in this case, electrodes) function as expected.
They consist of standard methods and protocols for detecting irregularities in performance.
Most external regulatory or accreditation agencies (e.g., Joint Commission for the Accreditation of Healthcare Organizations [JCAHO], Clinical Laboratories Improvement Amendments [CLIA]) demand internal quality monitoring.
• No particular instructions for routine calibration can be supplied due to the many varying processes, designs, and recommendations of various manufacturers. Therefore, operators must follow the manufacturer's guidelines to the letter.
Article Contributed By:-